
Anyone who ever had the pleasure of dealing with a yeast infection knows that it’s actually no pleasure at all. Candida albicans (C. albicans) is one of the most common human fungal pathogens that can cause such an undesirable yeast infection. Even though Candida can lead to a variety of diseases affecting different tissues in the body, vaginal infections are the most common ones. In fact, they affect up to 75% of the women at least once in their lifetime [1].
What many people don’t know is that Candida albicans is essentially a “friendly” commensal – meaning that it’s lingering on various mucosal surfaces in our body like our gut and mouth without the intention of doing us any harm. It is estimated that 30-70% of us provide a cozy home for Candida [2].
But, like so many things in life, the situation can go downhill quickly: if cell barriers are disrupted or the immune system is impaired, the formerly friendly fungi can start to grow uncontrollably and thus can promptly evolve into an irritating and uncomfortable experience. Diseases vary from common superficial mucosal complaints to not as common life-threatening systemic disorders as the presence of Candida in our bloodstream can trigger a septic shock, with a mortality rate as high as 50% [3].
Candida albicans: A Professional Shapeshifter
Candida literally exists in all shapes and sizes – and that’s one of the things that makes this fungal pathogen extraordinary and perilous at the same time. You could call it an intelligent super pathogen if you will: It has the ability to adapt in order to avoid the surveillance system of our immune cells and to disseminate through the host. From a rounded yeast cell, the fungus can easily transform into an elongated hyphal cell that is able to permeate the gut lining and colonise other tissues in the body.
In addition, the opportunistic yeast is also highly metabolically flexible, meaning it can utilise different nutrient sources for energy. So, in a nutshell, it will hardly ever go hungry and can easily survive different environments and conditions in distinct niches in the body. All these characteristics make a Candida infection or candidiasis both hard to diagnose and treat.
Common symptoms of Candida overgrowth
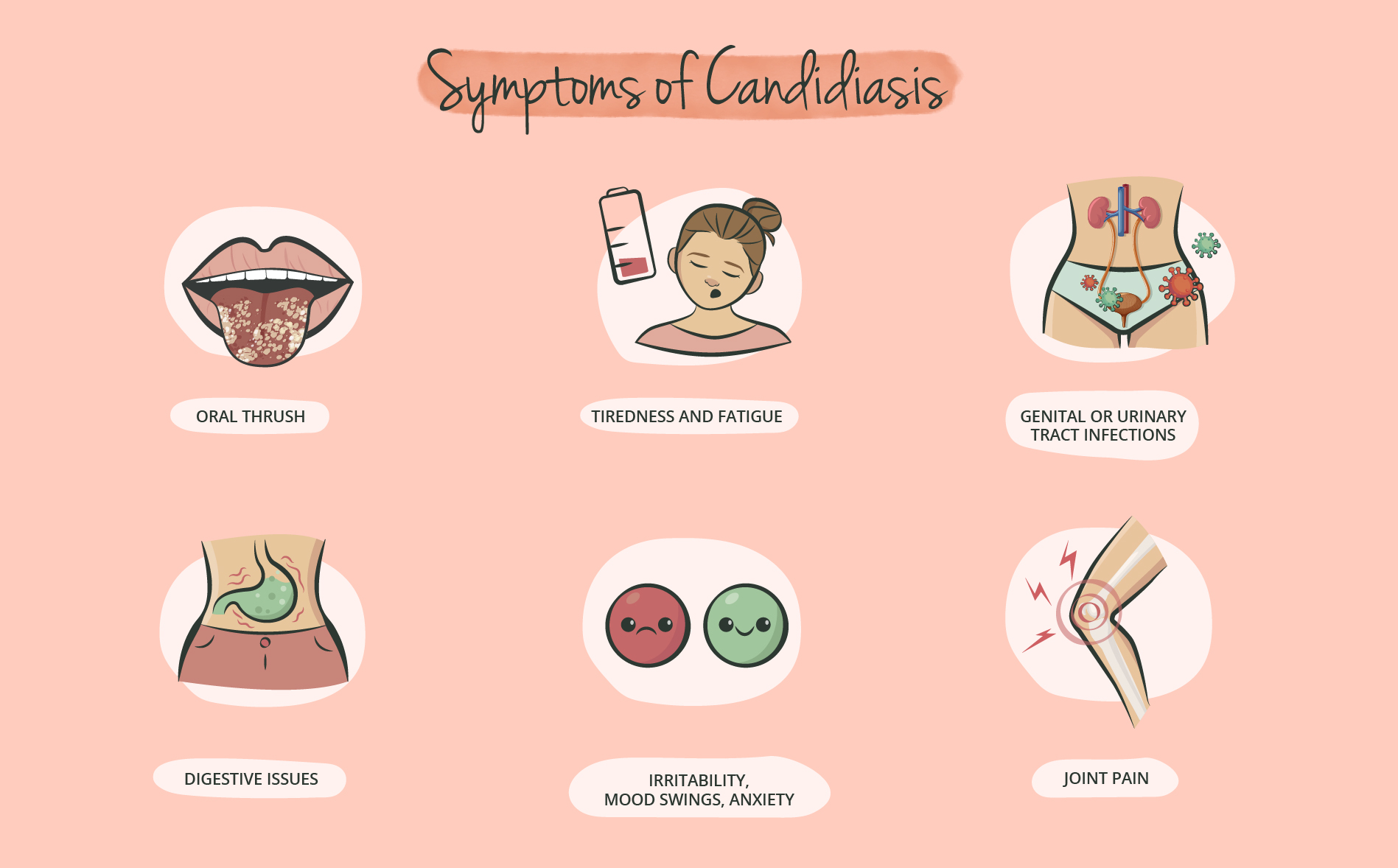
Another striking feature of Candida albicans is its ability to form biofilms, densely packed layers that adhere to mucosal tissues. These biofilms are visible for example on the tongue as white patches- referred to as oral thrush. That’s actually where the fungus got its name from: The Latin word candidus, means ‘gleaming white’; and albicans comes from albi-care, which translates to ‘to whiten’.
Candida overgrowth can be experienced in various forms nearly anywhere in the body. Other than the mouth, Candida albicans also commonly colonises the skin, ears, reproductive organs and even the thyroid. Hence, symptoms vary depending on the location of Candida overgrowth, ranging from constantly feeling worn down, digestive issues such as bloating and constipation, to skin eczema. Vaginal candidiasis is usually accompanied by vaginal itching and swelling.
Risk factors for a Candida infection
As mentioned, Candida albicans lives side by side with other commensal microorganisms in our body and normally doesn’t cause any trouble in healthy individuals. However, there are certain factors that can contribute to its overgrowth. One frequently observed trigger is the use of antibiotics. Antibiotics do not only eliminate the bad bacteria but also those that keep yeast – like Candida – from growing out of control [4].
Alcohol is another prominent factor that is associated with candidiasis, as candida and alcoholism frequently occur together. On the one hand alcohol encourages the proliferation of yeast and on the other hand yeast overgrowth can result in cravings for alcohol – a vicious cycle. Moreover, alcohol has been shown to weaken the immune system [5], which also reduces our body’s ability to keep pathogens like Candida albicans in check.
Speaking of which - people with a weakened immune system from illness or medications are not only more susceptible to infections including candidiasis, they also are more likely to experience a more serious case of the disease. The same applies to diabetics: studies have shown that there was a strong association between high blood sugar levels or poor glycemic control and prevalence rates of Candida infection [6].
How to beat Candida: It’s all about lifestyle
Due to the polymorphic nature of Candida, its ability to adapt to different environments and the emergence of antifungal resistance [7], treating candidiasis remains a clinical challenge and the number of available anti-candida drugs is still limited.
Luckily, scientific studies have provided several alternative methods of reducing C. albicans colonisation, including dietary modifications. Popular interventions include the so-called “Candida Diet” which is a rather strict low-sugar, anti-inflammatory diet that aims to restore the balance of bacteria and yeast, promote intestinal integrity and health and eliminate the sugars that promote Candida overgrowth. The focus lies on non-starchy vegetables, some low sugar fruits, gluten-free grains, and fermented foods, whereas all sources of flour, sugar, alcohol, dairy, and yeast are removed.
Apart from diet changes, supplementation with certain plant-derived compounds can provide additional support. Based on the available scientific findings we developed our Candi-Aid Complex, a supplement that combines plant extracts, probiotics, and specific fatty acids. The highly dosed extracts from olive leaves, grapefruit seeds, black garlic, watercress, and oregano contain essential oils and other phytocompounds with strong anti-inflammatory and antifungal properties [8, 9, 10, 11]. The Caprylic acid from MCT oil was also found to be a highly potent anti-candida compound [12]. Last but not least, we added the probiotic strain Lactobacillus rhamnosus as it was shown to reduce hyphal elongation, a key virulence attribute [13]. Of course, our product should not be considered a shortcut to defeating Candida – it’s merely designed to act as an additional helping hand in the context of a “Candida cleanse” regimen. At the end, it all comes down to lifestyle choices
Sources
[1] Azie et al. Oral Ibrexafungerp: an investigational agent for the treatment of vulvovaginal candidiasis. Expert Opin Investig Drugs. 2020
[2] Gow & Yadav. Microbe Profile: Candida albicans: a shape-changing, opportunistic pathogenic fungus of humans. Microbiology (Reading). 2017
[3] Gudlaugsson et al. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis. 2003
[4] Bisschop, Merkus & Van Cutsem. The influence of antibiotics on the growth of Candida albicans in the vagina: an experiment with vaginal fluid. Europ. J. Obstet. Gynec. reprod. Biol. 1985
[5] Afshar et al. Acute immunomodulatory effects of binge alcohol ingestion. Alcohol. 2015
[6] Zomorodian et al. Prevalence of oral Candida colonization in patients with diabetes mellitus. J Mycol Med. 2016
[7] Anderson. Evolution of antifungal-drug resistance: mechanisms and pathogen fitness. Nat Rev Microbiol. 2005
[8] Hammer, Carson & Riley. Antimicrobial activity of essential oils and other plant extracts. J Appl Microbiol. 1999
[9] Zoric et al. Antifungal activity of oleuropein against Candida albicans - The in vitro study. Molecules. 2016
[10] Tsutsumi-Arai et al. Grapefruit seed extract effectively inhibits the Candida albicans biofilms development on polymethyl methacrylate denture-base resin. PLoS One. 2019
[11] Watson et al. The effects of oral garlic on vaginal candida colony counts: a randomised placebo controlled double-blind trial. BJOG. 2014
[12] Jadhav et al. The dietary food components capric acid and caprylic acid inhibit virulence factors in Candida albicans through multitargeting. J Med Food. 2017
[13] Graf et al. Keeping Candida commensal: how lactobacilli antagonize pathogenicity of Candida albicans in an in vitro gut model. Dis Model Mech. 2019
Recommended Product

Candi-aid Complex
Elimination of yeast infections usually involves antifungal medication. A natural supplement in combination with probiotics and a healthy lifestyle, avoiding sugar, alcohol and chronic stress may be just as helpful- our Candida Complex is completely natural.


